Diabetic Retinopathy Treatment
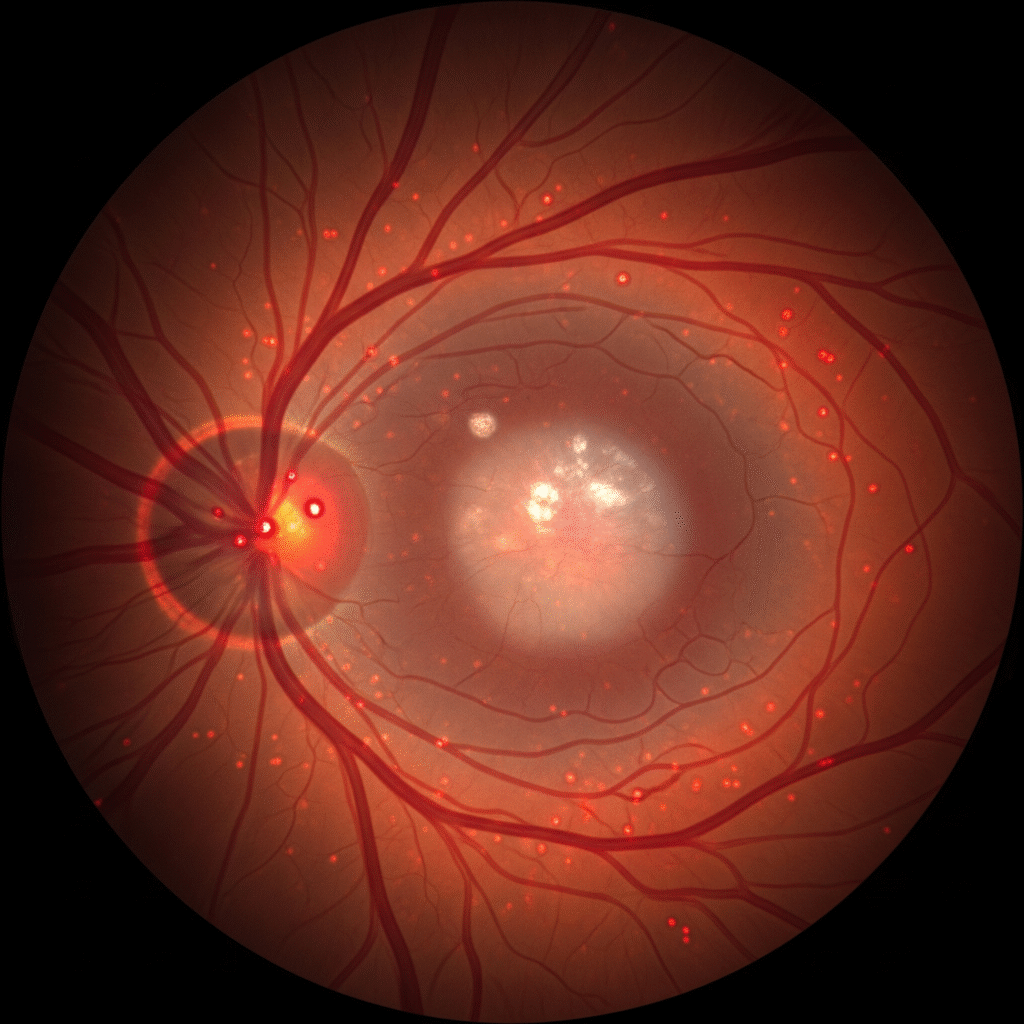
Diabetic retinopathy is a complication of diabetes caused by prolonged high blood sugar, which damages the retinal blood vessels. Treatment aims to slow disease progression and prevent vision loss.
In early stages (mild to moderate non-proliferative retinopathy), maintaining strict control of blood glucose, blood pressure, and cholesterol is essential. Regular retinal evaluations are recommended to monitor changes.
If diabetic macular edema develops, intravitreal injections of anti-VEGF agents (e.g., ranibizumab, aflibercept) are commonly used to reduce swelling and preserve vision. Corticosteroid injections or implants may be used in select cases.
In advanced stages (proliferative diabetic retinopathy), abnormal vessel growth can lead to complications. Laser treatment (panretinal photocoagulation) helps prevent bleeding and retinal detachment. If vitreous hemorrhage or tractional retinal detachment occurs, vitrectomy surgery may be required.
Early diagnosis through routine eye exams significantly improves outcomes. With effective systemic control and timely ophthalmic intervention, vision can often be preserved.
